Adhesive Capsulitis (Frozen Shoulder) Physiotherapy
The “real name” of frozen shoulder is adhesive capsulitis, and this condition affects up to 5% of the population. It affects more in women than men, typically above 45 years old.
To add to this – out of 10 people who develops frozen shoulder in ONE shoulder, there’s a 20-30% chance they will develop frozen shoulder in the other shoulder as well.
Ugh.
Contents
What’s frozen shoulder aka adhesive capsulitis?
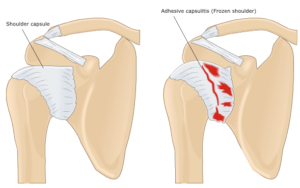
Basically it’s the stiffening of the shoulder and the shoulder joint because of scar tissue that forms and thicken. This causes painful shoulder movements and slowly decreases the amount of pain-free movements in the shoulder.
The annoying thing is that research hasn’t fully concluded what’s the actual cause of frozen shoulders, and the most commonly debated causes are
- Inflammation eg lining of a joint becomes inflamed (synovitis)
- Autoimmune reactions, where the body launches an “attack” against its own substances and tissues.
- Reactions after an injury or surgery
- Pain from other conditions, such as arthritis, a rotator cuff tear, bursitis, or tendinitis, that has caused a person to stop moving the shoulder
- Immobilization of the arm, such as in a sling, after surgery or fracture
What does frozen shoulder feel like?
Generally, patients with adhesive capsulitis has a classic tell-tale sign of
- gradually worsening pain
- gradually stiff shoulder
There are four stages of frozen shoulder:
Stage 1: “Prefreezing” Stage
Pain is the #1 feature of this stage; and unfortunately you may experience shoulder pain during day and at night.
To be frank, at this early stage, it’s often hard to know for sure if you have frozen shoulder, because at the beginning, it’s mild tightness and pain…which can be attributed to many many other conditions or injuries (such as a simple shoulder sprain).
Patients may experience shoulder pain and stiffness symptoms for up to 3 months, and it seems to not get better even with time. The shoulder aches even when it’s not moving or being used, and the shoulder pain has begun to become sharper rather than dull.
You may find yourself protecting your shoulder by using it less and using the other hand and shoulder more (this is a standard sign, called guarded movement).
You’d notice the decrease of shoulder movement in external rotation (external rotation is the movement where you turn your shoulder clock-wise outwards from your body, for example reaching out to receive change/coins). Mostly it affects movements when raising hands or reaching behind your back.
Stage 2: “Freezing” Stage
Stage 2 is marked with shoulder tightness and pain.
This stage typically is when you have had frozen shoulder symptoms and discomfort for 3 to 12 months. Over the months, your shoulder would have gradually become stiffer, resulting in
- decreased active range of movements
- pain (even at rest…and at night).
Your shoulder isn’t completely stiff, with some range of movement still available.
Stage 3: “Frozen” Stage
Stage 3 is the stiff shoulder stage and painful shoulder with movement
At this point, your adhesive capsulitis would have been around for 9 to 15+ months, and your shoulder would be pretty stiff by now, with greatly decreased range of shoulder motion.
Typically the shoulder pain would have dipped quite a bit, with “only” shoulder pain present when you actively move your shoulder joint.
Stage 4: “Defrosting / Thawing” Stage
This is the best stage where you start to regain shoulder movement and strength
Stage 4 of frozen shoulder is usually around months 12-24+, and the best is there is a significant decrease in shoulder pain especially at night. Most patients report that they can finally sleep without having the frozen shoulder pain waking / keep them up.
Of course, you may still have a limited range of movement in your shoulder, but you will experience both
- rapid improvement in overhead shoulder movements
- more confidence in moving and using shoulder more and more (without fear of shoulder pain and tightness)
How do you diagnose frozen shoulder?
Most of the time, an experienced doctor can diagnose your frozen shoulder fairly conclusively and quickly based on signs and symptoms alone; but sometimes they may call for specific imaging such as
- x-ray
- ultrasound imaging or
- MRI
to rule out other potential shoulder problems such as fractures, ligament tears etc.
The doctor will also examine you and ask you to move your shoulder and arm in specific ways to check for pain and see how far you can move your shoulder (active range of motion or AROM for short). Then they will ask you to relax your muscles and joint whilst they move your arm to check for your passive range of motion (PROM).
Then they will look for a specific patterns in your shoulder’s decreased range of motion called a “capsular pattern” that is typical with frozen shoulder. In addition, we have to also consider other conditions you might have, such as
- diabetes
- thyroid disorders
- autoimmune disorders
that are associated with adhesive capsulitis.
Many patients who develop frozen shoulder typically go for shoulder physiotherapy in the second or even third stage (simply because they usually dont know what it is and thought it’d go away…by 12-24+ months is a long time). Physiotherapists will perform a thorough shoulder examination and evaluation, including an extensive health history, to rule out other diagnoses.
How physios can help with frozen shoulder
Physiotherapist’s overall goal is to restore your movement, so you can go back to
- sports & playing stuff you enjoy
- work & responsibilities
Once the evaluation process has identified the stage of your condition, the physiotherapist will create an individualized exercise program tailored to your specific needs. Exercise has been found to be most effective for those who are in stage 2 or higher. Your treatment may include:
Stages 1 and 2 frozen shoulder physiotherapy
- Gentle stretches, manual therapy & careful exercises. This is to maintain as much range of motion as possible and will help reduce your pain.
- Modalities. Your physical therapist may use heat therapy and cold therapy treatments (modalities) to help relax the muscles prior to other forms of treatment.
- Pain medication. Sometimes, conservative care cannot reduce the pain of adhesive capsulitis. In that case, your physical therapist may refer you for an injection of a safe anti-inflammatory and pain-relieving medication. Research has shown that although these injections don’t provide longer-term benefits for range of motion and don’t shorten the duration of the condition, they do offer short-term pain reduction.
Stage 3 frozen shoulder physiotherapy
Physio goal of phase 3 is on the restoring natural and full shoulder motion. Treatment may include:
- Stretching out the shoulder joint and soft tissues in and around the shoulder to restore shoulder movement and flexibility.
- Manual therapy is useful to go deep into soft tissues to loosen them up before any forms of stretching and shoulder exercises
- Strengthening. You may begin strengthening exercises targeting the shoulder area as well as your core muscles. Your home physiotherapy exercise program will change to include these exercises.
Stage 4 frozen shoulder physiotherapy
Here is the final stage of frozen shoulder, and your physio will focus on full restoration of normal shoulder movement, stamina and strength; goal is pain-free shoulder.
Treatments here are similar to the ones in stage 3 above be it stretching, manual therapy and strengthening; just kicked up a few notches. Of course, the physio may work on return-to-work or return-to-sport customized program for you.
Where To Next?
- Go to Home / Start
- Learn and find out more about your pains (bones, muscles, joints, tendons, ligaments, nerves etc) at Pain Conditions & Injuries
- Visit our shop to see products we recommend for pain relief, heating, treatments and more
- Contact us






