Below-knee Amputation Physiotherapy
Sometimes individuals have to have a grueling decision to amputate below the knee, be it due to disease, congenital defect or trauma; and it tends to be a life-or-death situation. Below knee amputations make 23% of all lower limb amputation and tends to be highest in people above 65 years old.
Contents
What’s a below-knee amputation?
Medically shortened to “BKA”, it’s a surgical procedure performed to remove the lower limb below the knee (typically just below the knee) when that limb has been severely damaged or is diseased and poses risks to health and life.
That being said, most BKAs, around 60-70% are due to peripheral vascular disease or diseases affecting circulation in the lower limb.
Poor circulation will decrease healing rate and immune responses to injury, increasing chances of foot or leg ulcers. Poor circulation may also decrease healing of these ulcers that may lead to infections that can spread to bone and become life-threatening.
Amputation is always a last-line of decision and done to remove the diseased tissue and prevent the further spread of infection, and to save life.
The need for below-knee amputation is caused by conditions including:
- Peripheral vascular disease (poor circulation)
- Diabetes
- Infection
- Foot ulcers
- Trauma causing the lower leg to be crushed or severed
- Tumors
Transtibial amputation surgery is usually done by an orthopedic surgeon – the diseased or severely injured part of the limb is removed, and the doctor will always try their best to preserve and keep as much of the healthy limb as possible, as well as shape the remaining limb to allow the best use of a prosthetic leg after recovery.
How physiotherapy can help
Before to below knee amputation surgery
- exercises for preoperative conditioning, and to improve the strength and flexibility of the hip and knee
- teach you how to walk with a walker or crutches
- educate you about what to expect after the procedure
Immediately after surgery
Most patients stay 1-2 weeks in the hospital after the surgery, to make sure the wounds heal well and no medical issues before returning home. You will notice a medical drain to drain out fluids and blood during your hospital stay.
You will be on medication and painkillers on the short term.
Patients will typically start physiotherapy as soon as possible, even on the day itself or latest the next day after surgery at your bedside.
Your first 2 to 3 days of treatment may include:
- Gentle stretching and range-of-motion exercises
- Learning to roll in bed, sit on the side of the bed, and move safely to a chair
- Learning how to position your surgical limb to prevent joint stiffness and joint contractures (the inability to straighten the knee joint fully, which results from keeping the limb bent too much)
When you are medically stronger and stabler, the physiotherapist will help you learn to move about in a wheelchair, and stand and walk with an assistive device such as crutches or walking frame
Below-knee amputation physiotherapy
The physios will help you fit your prosthesis and guide / train you to build your strength, stability and stamina for maximum movement and function.
Your treatments may include:
Prevention of joint stiffness and contractures
The #1 problem with any injuries and post-surgery is stiffness and contractures. They basically refer to soft tisssue tightness that can deveop that will make it very difficult to move, and happens due to
- lack of movement especially from end-range to end-range
- prolonged (too much) rest or even avoidance of use
The most common contracture after a below knee amputation is the knee and/or hip becoming flexed and difficulty or inability to straigthen. This cannot be allowed to happen, because it can become permanent (non-reversible) and that will make it very if not impossible to move properly again.
The physios will help you build and maintain good range of motion and posture at your knee and hip; as well as how to position your limb to prevent contractures plus stretching exercises to ensure the range is always good.
Compression to reduce swelling and shaping the stump
It is very normal to have swelling after any injury, and especially after surgery.
There are ways to maintain safe and constant compression to help reduce the swelling as well as doubling to shape the stump, using elastic bandages and an elastic shrinker sock. You’ll want a nice rounded stump to fit nicely into the stump, for highest fit and comfort (prevents pressure sores too).
Pain management
There will be aches, pains and discomfort, and physiotherapy can use the following to help manage the pain
- Manual therapy such as soft tissue (ie, muscle, tendon) mobilization, joint manipulation, gentle range-of-motion exercises, in order to improve circulation and joint movements
- Desensitization physiotherapy to help modify how sensitive an area is to clothing, pressure, or touch (after a wound heals, the scar can become very sensitive even to mild touch or pressure).
- Mirror therapy and/or graded motor imagery
80% of people who undergo amputations experience a phenomenon called phantom limb pain, a condition in which some of their pain feels like it is actually coming from the amputated limb. There are physiotherapy treatments that can help.
Prosthetic fitting and training
A prosthetist will be activated to customize a prosthesize (a walking device that is suited to your stump) to help you return as much as possible to normal activity and life.
You may get a temporary one at first as your stump heals (which will shrink) over 6-12 months, and your final prosthesis will be modified to fit you as you needs may be.
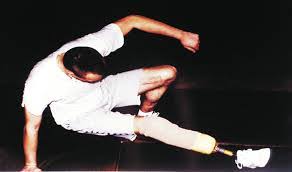
Good news is that most individuals with below knee amputations will learn to move and walk well with a prosthesis. Some even run with it!.
Functional training
After you move from acute care to rehabilitation, you will learn to walk, move and function more and more independently – the goal is for you to be self-independent and not need to rely on anyone for you to move about where possible.
You will first learn about wheelchair mobility, and then leveled up to prosthesis walking, with or without crutches.
You will also learn about
- successful use of your new prosthetic limb
- how to care for your residual limb with skin checks and hygiene
- continued contracture prevention with exercise and positioning
- putting on and taking off your new prosthesis
- how to manage a good fit with the socket type you receive
Where To Next?
- Go to Home / Start
- Learn and find out more about your pains (bones, muscles, joints, tendons, ligaments, nerves etc) at Pain Conditions & Injuries
- Visit our shop to see products we recommend for pain relief, heating, treatments and more
- Contact us




