Dementia and Alzheimer’s Disease Physiotherapy
At least 5% of people above 60 years old; and 40% of people above 85 years old have Alzheimer’s disease. This means that they will have to live with problems such as loss of memory, speech, ability to do tasks or even basic activities of daily living.
Physiotherapists can help by working with families and caregivers to help keep patient as active as possible, moving safely; and this will slow down the worsening of dementia.
Contents
First off: what’s dementia?
Often used interchangeably with the term Alzheimer’s disease, it’s a gradual worsening condition that damages brain cells. It will affect how we think, how we speak, how we interact with others and our environment (tasks, work, responsibilities, hobbies etc).
To be specific: dementia is a general term, whereas Alzheimer’s disease is a specific brain disease. Dementia is marked by symptoms that gradually get worse over time. Alzheimer’s disease first affects the part of the brain associated with learning, so early symptoms often include changes in memory, thinking and reasoning skills.
20% of deaths in adults above 65% is accounted to Alzheimer’s – a lot. That’s 1 in 5. The other causes are
- cancer
- stroke
- heart disease
- accidents
- respiratory disease
To make matters worse, the risk of getting Alzheimer’s disease increases with time and age…but it’s rarer / unusual to get dementia before age 60. And yes, if your relative has it, that increases your chances of getting it somewhat, but even people whose family dont have it can get it too.
Signs and symptoms of dementia and alzheimer’s

One of the biggest signs is confusion. Yes, even if there are other potential causes of confusion for example history of head injuries or infections, but can be treated.
10 important warning signs of possible Alzheimer’s disease:
- Changes in mood or personality
- Misplacing items and losing the ability to retrace your steps
- Finding the right words to say when speaking or writing
- Confusion about time and or place
- Difficulty completing familiar tasks
- Difficulty making decisions, especially in planning or solving problems
- Memory changes that disrupt daily life
- Trouble understanding visual images or the way things physically fit together (spatial relationships)
- Poor or decreased judgment about safety
- Withdrawal from work or social activities
A common sign is people getting “lost” or confused in places that they were familiar with before, even frequented ones.
Later stages of dementia, they may develop “sundowning”, where they get restless and wander and get lost. Often they are then brought back by police. Sometimes they start to not speak to their family members or friends; and worse, they may see or hear things that didn’t happen or aren’t there at all. A common theme is that they may falsely believe that others are trying to harm, cheat or lie to them (that’s why many often have fights with their family and friends).
On top of those, there’s more – people with alzheimer’s may gradually find it difficult to do basic living tasks, and eventually will need help with
- feeding / drinking
- changing
- toileting
- bathing
- etc
Only at the last stage of dementia would the patient start to lose their physical ability to walk…but usually because of confusion, safety and security issues, people with alzheimers will very, very likely need to have assistance or supervision to get around.
How do we diagnose Alzheimer’s Disease?
So it’s not so easy to diagnose alzheimer’s, simply because the exact cause is unknown (may be caused by multiple factors over different periods of time). What’s happening is that researchers tend to diagnose using brain imaging studies such as
- computed tomography scan
- magnetic resonance imaging (MRI)
- positron emission tomography (PET) scan or
- ultrasound
These tests can show abnormalities in brain structure or function.
Patients may also be made to perform other tests such as
- mental function tests
- cerebral spinal fluid tap
- biomarker
- genetic testing
The most accurate diagnosis can be made only on autopsy, but of course we cant do that on a living person at all.
Physiotherapists may play an important and integral role in recognizing early signs or symptoms of dementia. If they recognize you or your loved one may be showing signs or symptoms that’s consistent with dementia or Alzheimer’s, they will help refer you to a suitable specialist to help.
How physiotherapy can help with alzheimer’s
For patients with Alzheimer’s disease, research shows that physical activities and exercise may (and does) help with / to
- improve memory
- delay the onset of dementia and Alzheimer’s disease
- slow the decline in ability to perform activities of daily living in people who have Alzheimer’s disease
Physios can help to keep patients active, fit and mobile; which can help them continue to engage in their basic living roles as well as roles in their homes and community. In later stages, help decrease caregiver burden by keeping patients strong/active as possible as well as train caregivers how to manage a patient with dementia.
It may help improve quality of life and also possibly delay the need for long term warding in hospitals or nursing home.
That being said, people with Alzheimer’s disease may also develop other conditions related to aging, such as arthritis and osteoarthritis, have falls, bone fractures such as hip fractures and spine fractures etc which all will need the help of physiotherapy.
Dont worry, the therapist will likely use various teaching approaches, techniques to simplify instructions, and unique approaches, including:
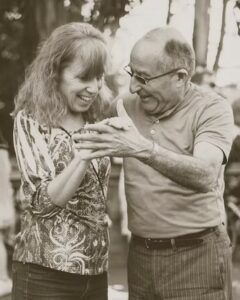
- Visual, verbal, and tactile cueing – using cues such as pointing to objects or gesturing in case verbal instructions are difficult. Eg patting on the chair if we want the patient to sit on that particular chair. Cues can also be given verbally with short, simple one-step instruction. Tactile clues such as holding someone’s hand to have them walk with you.
- Mirroring – With this technique, we serve as a “mirror,” standing directly in front of the person to show them how to move. To help the person raise his or her right arm, the therapist’s left arm would be raised.
- Task breakdown – breaking down tasks into shorter, simple “pieces” to be completed one step a time is helpful for many patients. Example, if the physio wants to teach a person how to safely move from lying in bed to sitting in a chair, the therapist might have the person practice rolling to the side, then pushing up to sitting, before pivoting into the chair.
- Chaining – step-by-step instructions to link steps together in a more complicated movement pattern. This technique usually is used once task breakdown has been successful and unites the separate steps of moving from lying in bed to sitting in a chair, to make it one fluid movement.
- Hand over hand facilitation – We take the hand or other body part of the person who needs to move or complete a task and moves that body part through the motion.
Although people with Alzheimer’s disease usually maintain the ability to walk well into the late stages of the disease, balance and coordination problems often lead difficulties in
- balance / stability
- walking / gait pattern
- flexibility
Physios will train these “walking” muscles to learn to respond to changes in the environment, such as uneven or unstable surfaces, on a movement pattern level.
Train caregivers on how to take care of their loved ones safely
It’s not only a big change for patients with dementia or alzheimer’s, it’s also a very big change for the patient’s family, with a lot of things to adapt to. The patient is no longer the same as before, and will gradually worsen over time.
The family and caregiver will definitely need training and instruction on how to care for the patient with alzheimer’s at different stages of the disease, from beginning, middle to late stage; factoring in how to include as much activity safely for the patient to maintain as much function and movement (helps to slow down progressive worsening) vs helping/not overhelping.
The ideal is the maintenance of patient’s dignity, memory, movement and function as much as possible.
Where To Next?
- Go to Home / Start
- Learn and find out more about your pains (bones, muscles, joints, tendons, ligaments, nerves etc) at Pain Conditions & Injuries
- Visit our shop to see products we recommend for pain relief, heating, treatments and more
- Contact us




